Written by Smita Sen
+
Illustration by Yo-Yo 
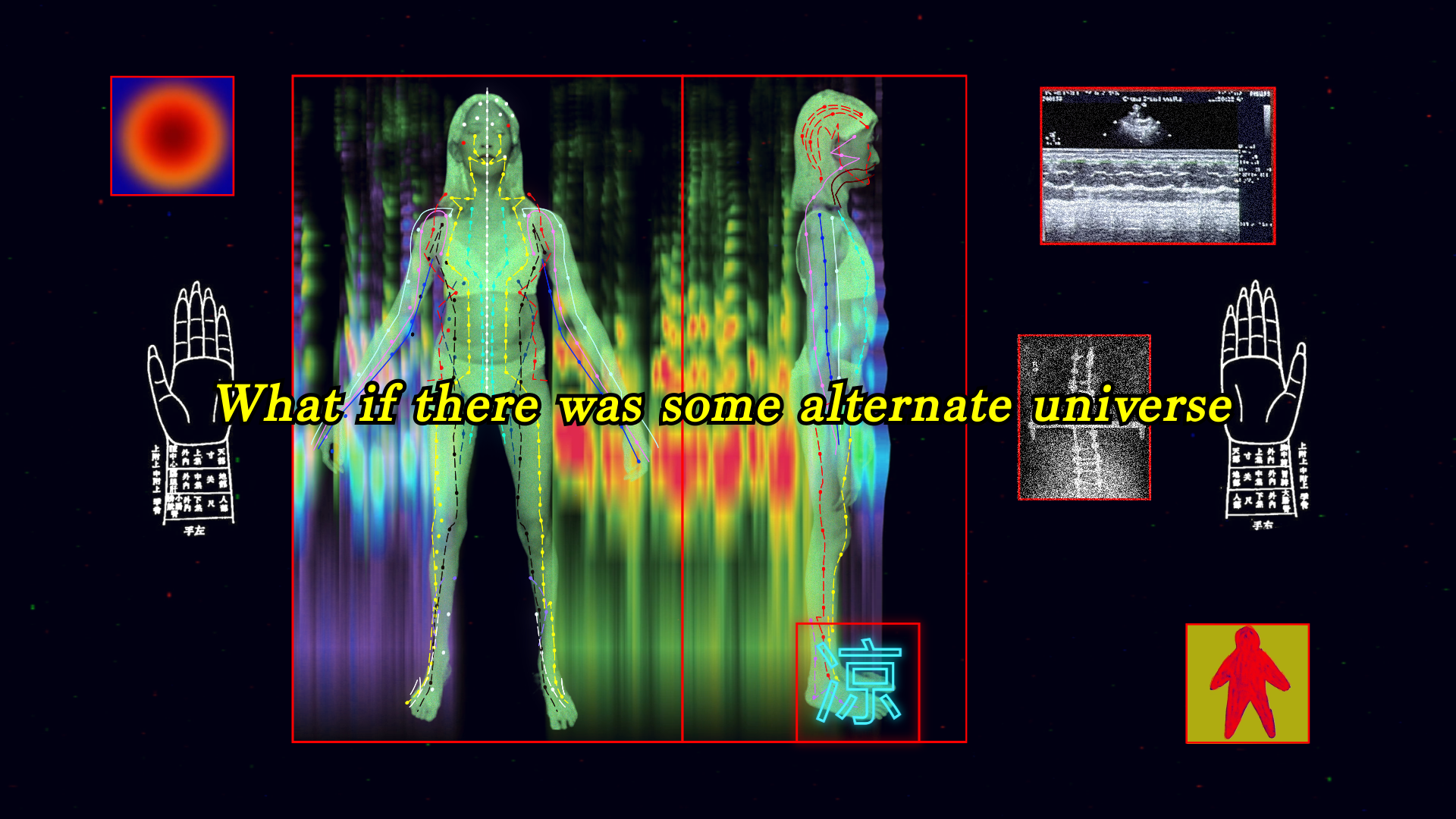
Still from Re:collections
In this article, I hope to bridge the recent medical literature with my personal narrative as a palliative caregiver to my father. In doing so, I hope to expand the discourse on digital media, caregiving, and grief, offering a meditation on the deeply felt impact of this time on our society.
Limbo
I often find myself walking through each day numb to my surroundings. I hear in my mind the metronome of limbo: the endless drone of machines beeping in the hospital; the nurses’ intercom; the life support keeping my father alive and dead at the same time. In my moments of uncertainty, I return to the hospital in my mind. Somehow, it brings me peace. Hospitals are the intermediary space that cradle all life hanging in the balance – the living and the dying, the ill and the recovering, the newly born and the slowly lost.
For the entirety of the COVID-19 pandemic, we have been living in suspended rupture. As visiting restrictions reached paramount levels at hospitals and nursing homes, we have been largely cut off from hospitals, from these vital intermediary spaces. Increased visiting restrictions have meant that the rituals of caregiving and grief have shifted – we care for our sick loved ones over FaceTime and conduct our memorial services over Zoom. Though these digital tools have been crucial in this time of isolation, I have often asked myself: Are these tools enough? What happens when we are separated from our loved ones in their hour of greatest need?
Doctors, nurses, and medical researchers have been asking the same questions.From the early months of the pandemic in 2020, the World Health Organization (WHO) recommended that “numbers of visitors and visiting periods should be highly restricted” at hospitals, nursing homes, and other medical facilities (WHO 2020, p.10). The realities of increased visiting restrictions have troubled healthcare practitioners. In 2021, the International Journal of Nursing Studies published a comprehensive study of the impact of heightened visiting restrictions due to COVID-19 policies. In this study, researchers Hugelius, Haruda, and Marutani analyzed seventeen research papers covering medical facilities in fourteen countries. 1 Across the board, the results showed a consistent trend: that the increased visiting restrictions had largely negative impacts on patient survival and psychology; on caregiver well-being; and on doctors and nurses themselves.
These negative impacts are not difficult to imagine. Without their loved ones nearby, patients would often eat less and engage less in activities of daily living. They reported experiencing greater pain and increased physical symptoms, as well as loneliness, agitation, and depressive symptoms (Hugelius, et al., 7). In times of illness, loved ones take the edge off the pain, and often, play a pivotal role in patient recovery and survival (Walker, et al., 404; Seppala, et al., 417-418). The ritualistic care provided by family caregivers to sick loved ones in the hospital or hospice – waking up with them, helping them with their medications and meals, emotionally preparing them for treatments, both invasive and non-invasive – are a vital part of healthcare and the patient recovery process. Without visitors by their bedside, patients have struggled through the pandemic. In many ways, patients’ experiences are mirrored by those of their loved ones. Separated from a patient, family caregivers have experienced intense anxiety and have reported lower scores for their psychosocial well-being (Hugelius, et al., 7). In medical facilities across the world, the results were consistent: separated by visiting restrictions and living in isolation, patients and their loved ones experienced heightened levels of physical and psychological pain.
This feels like an intuitive outcome. In my gut, it makes sense. If I wasn’t there to hold my father’s hand as he suffered through treatment after treatment, would I ever forgive myself? With only a Zoom call, would he have felt comforted, loved, secure? The rituals of caregiving are not rote and easily digitized. They require moments that are intangible and difficult to replicate – hands held upon waking from general anesthesia; the whisper of a memory or a joke; the humming of a lullaby as nurses replace the central line. These tiniest gestures, these minute rituals of caregiving, are in many ways foundational to the way we relate to one another. When faced with illness and mortality, it is the hands holding us that ensure we feel comforted and secure. It is in paying close attention to our loved ones that we honor our interdependence — in picking my father up when he had fallen down; in holding him upright when he walked to the bathroom; in joking with him as we would check his oxygen levels. These rituals do more than offer comfort in times of illness and fear. For both patient and caregiver, these rituals of care can reaffirm the essence of our humanity.
Among the images most emblematic of this complicated period in our history are those of nursing home visits. During the first peak of the COVID-19 pandemic in early 2020, many elderly patients in nursing homes were cut off from outside contact. There are countless photographs of visitors – children, grandchildren, partners, siblings – pressing their hands and faces to nursing home windows, attempting to come as close as physically possible to their aging loved ones. Another one of our most vital end-of-life caregiving rituals, spending time with our sick elders in the last years, months, weeks of their lives, had been disrupted. By June 2020, the seclusion of the elderly became one of the most hotly debated policy issues across the world. When Belgian Prime Minister Sophie Wilmes announced a loosening of restrictions to permit one visitor per nursing home patient, there was grave concern and well-founded criticism. Critics emphasized that the most vulnerable elderly will be put at greater risk and that the spread of infections could endanger both the sick and care workers. Marc Bourquin of the Hospital Federation of France responded with the opposite concern, “We cannot condemn these people to never see their loved ones again” (Casert and Charlton, 2020). Government officials and leaders in public health across Europe were weighing in on these most essential questions: Can we keep each other both safe and loved? What can we do both to be safe and to ensure that no one has to live their last moments alone?
My aging loved ones, my elderly aunts and uncles with complicated medical histories, were also self-isolating at home in countries far away. I prayed for their survival, for the chance to see them again soon. It was at this time, early 2020, that my mother and I were living together under lockdown. Time became strange, at once too slow and too fast. I would sit numbly flipping through news stories. We received phone calls about friends and family who passed away alone in the hospital. I found myself looking intently at my loved ones over FaceTime and Zoom. Are you really there? Am I really here? Each moment of contact seemed to bring back that most universal fear. If we are digitally together, will we never have to die alone?

Still from Re:collections, image by Yo-Yo Lin
Sanctuaries
I wonder often if digital technologies can hold us together. Since the widespread adoption of the internet in the 1990s and 2000s, there has been an interest in the ways we navigate the most sensitive parts of human existence with digital technologies–illness, end-of-life care, and grief. These questions have become paramount in the COVID-19 pandemic, where we are dependent on isolation, virtual memorials, and digital caregiving to ensure our collective safety.
The initial examinations of grief, care, and the internet consider the healing potential of virtual memorials. In a 2009 article examining the online grief rituals on MySpace, media scholar Robert Dobler compares virtual memorials to roadside memorials. He contemplates both as sites of public memorialization that serve as safe havens for one’s private grief. In a Scientific American Mind article published in 2013, psychologists and health professionals similarly consider how Facebook had become a new space for gathering, mourning, and other rituals of collective grief. In the wake of one’s passing, a dedicated web page or social media profile becomes a place for videos, photographs, memories – mementos of grief shared across time zones and borders. Cyberspace becomes a grieving space, and, in so doing, can serve as a community gathering place. The Scientific American Mind article describes the role of such virtual memorials well: “Like holding a wake or sitting shivah, a virtual memorial provides the bereaved with social support, a sense of connection with both the deceased and the living” (Arnold, 23). Like the roadside shrines described by Dobler, the virtual memorial has become a site of shared sanctuary for all of us to remember our loved ones and to acknowledge our grief. In the midst of the COVID-19 pandemic, the virtual memorial has become one of our primary modes of expressing collective grief, for better and for worse.
The gift of the virtual memorial is accessibility and permanence. A virtual memorial can be accessed by loved ones around the globe at any time of day. The challenge of the virtual memorial lies in our physical separation. How much closure and community support can we have in the grieving process if our only understanding of the loss exists online? Other digital tools have come in to fill some of these gaps. Video conferencing and livestreamed funerary services have seen a sharp rise in popularity, allowing those who have shared a loss to gather safely in the digital sphere. 2 With these services, some elements of communal grieving can be recreated virtually.
Still, the realities of physical separation become more pronounced in end-of-life care and limited hospital visitation. It is in these arenas where digital technology has not yet begun to meet our socioemotional needs at the end of life: togetherness, affection, physical touch, closure. Medical researchers have expressed concerns over the long-term impacts of this time when millions have spent their last moments alone and countless loved ones were never able to say goodbye. 3 If being away from each other in our greatest hours of vulnerability is what will keep us collectively safer, how can digital technologies better replace the physical and psychological support made tangible by hospital visitation?
Answering this question, a number of medical research articles were published over the past two years examining the need for more sophisticated digital media, robotics, virtual reality tools, and haptic devices to accommodate the restrictions brought on by COVID-19. 4 In the article Manifesto for Digital Touch in Social Crisis, twelve Human-Computer Interaction and media researchers describe the need for more sophisticated haptic interfaces that can replicate human touch in this time of social isolation. The authors note that overwhelmingly, current haptic interfaces rely on only one sensation: binary on-off vibratory feedback. They acknowledge and encourage the development of haptic technologies that “enrich digital social touch interactions and embed other input modalities such as force, shear, twist, and squeeze” (Jewitt, et al., 6). Such technologies could potentially begin to offer the types of multisensory bedside interaction that isolated hospital and nursing home patients need. These digital tools can begin to recreate one of the rituals of togetherness that bring ease to both patients and their caregiving loved ones.
Yet, such technology is only nascent at best. What remains to be seen is when these digital tools are produced, will they be democratized and made available for reproduction around the world? Or will they be hoarded by wealthy nations? Will these technologies be developed in a way that honors the global need for sustainability in design and manufacturing? Or will the immediacy of our needs outweigh the future of our planet? And, last but not least, would these technologies even work? If we could produce haptic devices that could recreate complex touch, would they provide the same levels of comfort and security as having a loved one by your bedside? Could the warmth of one’s pulse and the tightening grip of a loved one’s hand be replicated effectively? And even if technology could do so, how much would be missing? If the rituals of bedside caregiving are made of the intangible—tenderness and attention, sharing memories, brushing one’s hair as they wake from general anesthesia—could digital technology ever fully replicate these vital rites?
For moments that are precarious, moments as fragile and irretrievable as the last minutes of a life, it feels difficult to suggest that digital media could suffice. And yet, it will have to. With this time of widespread contagion, overloaded hospitals, and isolation, digital media is one of the only options to care for our loved ones in their times of illness. It is only through virtual sanctuaries that most of us can carry our loved ones from this world into the next.
Sanctuaries
I wonder often if digital technologies can hold us together. Since the widespread adoption of the internet in the 1990s and 2000s, there has been an interest in the ways we navigate the most sensitive parts of human existence with digital technologies–illness, end-of-life care, and grief. These questions have become paramount in the COVID-19 pandemic, where we are dependent on isolation, virtual memorials, and digital caregiving to ensure our collective safety.
The initial examinations of grief, care, and the internet consider the healing potential of virtual memorials. In a 2009 article examining the online grief rituals on MySpace, media scholar Robert Dobler compares virtual memorials to roadside memorials. He contemplates both as sites of public memorialization that serve as safe havens for one’s private grief. In a Scientific American Mind article published in 2013, psychologists and health professionals similarly consider how Facebook had become a new space for gathering, mourning, and other rituals of collective grief. In the wake of one’s passing, a dedicated web page or social media profile becomes a place for videos, photographs, memories – mementos of grief shared across time zones and borders. Cyberspace becomes a grieving space, and, in so doing, can serve as a community gathering place. The Scientific American Mind article describes the role of such virtual memorials well: “Like holding a wake or sitting shivah, a virtual memorial provides the bereaved with social support, a sense of connection with both the deceased and the living” (Arnold, 23). Like the roadside shrines described by Dobler, the virtual memorial has become a site of shared sanctuary for all of us to remember our loved ones and to acknowledge our grief. In the midst of the COVID-19 pandemic, the virtual memorial has become one of our primary modes of expressing collective grief, for better and for worse.
The gift of the virtual memorial is accessibility and permanence. A virtual memorial can be accessed by loved ones around the globe at any time of day. The challenge of the virtual memorial lies in our physical separation. How much closure and community support can we have in the grieving process if our only understanding of the loss exists online? Other digital tools have come in to fill some of these gaps. Video conferencing and livestreamed funerary services have seen a sharp rise in popularity, allowing those who have shared a loss to gather safely in the digital sphere. 2 With these services, some elements of communal grieving can be recreated virtually.
Still, the realities of physical separation become more pronounced in end-of-life care and limited hospital visitation. It is in these arenas where digital technology has not yet begun to meet our socioemotional needs at the end of life: togetherness, affection, physical touch, closure. Medical researchers have expressed concerns over the long-term impacts of this time when millions have spent their last moments alone and countless loved ones were never able to say goodbye. 3 If being away from each other in our greatest hours of vulnerability is what will keep us collectively safer, how can digital technologies better replace the physical and psychological support made tangible by hospital visitation?
Answering this question, a number of medical research articles were published over the past two years examining the need for more sophisticated digital media, robotics, virtual reality tools, and haptic devices to accommodate the restrictions brought on by COVID-19. 4 In the article Manifesto for Digital Touch in Social Crisis, twelve Human-Computer Interaction and media researchers describe the need for more sophisticated haptic interfaces that can replicate human touch in this time of social isolation. The authors note that overwhelmingly, current haptic interfaces rely on only one sensation: binary on-off vibratory feedback. They acknowledge and encourage the development of haptic technologies that “enrich digital social touch interactions and embed other input modalities such as force, shear, twist, and squeeze” (Jewitt, et al., 6). Such technologies could potentially begin to offer the types of multisensory bedside interaction that isolated hospital and nursing home patients need. These digital tools can begin to recreate one of the rituals of togetherness that bring ease to both patients and their caregiving loved ones.
Yet, such technology is only nascent at best. What remains to be seen is when these digital tools are produced, will they be democratized and made available for reproduction around the world? Or will they be hoarded by wealthy nations? Will these technologies be developed in a way that honors the global need for sustainability in design and manufacturing? Or will the immediacy of our needs outweigh the future of our planet? And, last but not least, would these technologies even work? If we could produce haptic devices that could recreate complex touch, would they provide the same levels of comfort and security as having a loved one by your bedside? Could the warmth of one’s pulse and the tightening grip of a loved one’s hand be replicated effectively? And even if technology could do so, how much would be missing? If the rituals of bedside caregiving are made of the intangible—tenderness and attention, sharing memories, brushing one’s hair as they wake from general anesthesia—could digital technology ever fully replicate these vital rites?
For moments that are precarious, moments as fragile and irretrievable as the last minutes of a life, it feels difficult to suggest that digital media could suffice. And yet, it will have to. With this time of widespread contagion, overloaded hospitals, and isolation, digital media is one of the only options to care for our loved ones in their times of illness. It is only through virtual sanctuaries that most of us can carry our loved ones from this world into the next.

Still from Re:collections, image by Yo-Yo Lin
Metronomes
It is October 2021 and I am in a hospital again, the non-COVID section, this time as a patient. The monitors continue to beep the way they always have. The metronome of limbo is familiar and relaxing, the nurses calm and kind. I am waiting for a call but there is no service here. A friend sits by my bedside as I mentally prepare for the next set of tests. I had squeezed his hand in panic after getting stuck with needles four times in three different parts of my arms. It is a relief to have him here. It is a relief to know I have someone who loves me and understands me. Someone on my team.
The hospital allows one visitor, no alternates. If my friend needs to go home, no one else will be able to come to his place. I try hard to be compassionate, letting him know he can go home if he’s too tired. He’s kind and stays. I am grateful. I would be more afraid if he were not here. It would be more dangerous if he were not here. It is not my first rodeo, having been a palliative caregiver to my dad. I am used to hospitals, I bring my own blanket. My friend gets service on his phone. My mom calls and it’s nice to talk to her. I let her know that it’s not a big deal, really, and I’m going to be fine. I hold the phone after we hang up. If we are both gripping a phone, does this count as holding hands? I smile at my friend as we both try to get some rest.
I remember the hospital as a caregiver in a pre-pandemic world. My mother, brother and I served as my father’s full-time caregivers, we would sit together by my father’s bed. I remember my father feeling traumatized by the hospital. I remember the first time he was discharged from the hospital, arms bruised, body emaciated. He never wanted to come back. He would come back. We would lose him here. I lay in my hospital bed and feel grateful to have been with my father for every last moment. I feel grateful for the togetherness, for the chance to have my cousins and aunts and family friends sit with my father in the Intensive Care Unit. I feel gratitude and confusion and pain. The grief is always like that, never fully one feeling or another. I adjust my position on the hospital bed. I think about the fabric of the hospital gown and wonder about this other tactile sensation. Will you hold my hand? I feel the pulse of his heartbeat in my hands. The metronome of limbo is steady. Will you swaddle me with blankets from home? Can I have that sweater I love? If hospitals are where so many of us will leave this earth, can we leave with love and dignity? With our humanity intact? I look at my friend again, feeling grateful. I smile at him. He smiles back. Will you hold my hand?
Footnotes
1 In the cited article from the International Journal of Nursing Studies, the authors wrote that their research included data from (in no particular order) the United States, Saudi Arabia, Spain, Canada, France, India, the United Kingdom, the Netherlands, Italy, Taiwan, Hong Kong, Japan, Ireland, and Germany (Hugelius, et al., 3).
2 Zoom, the company that offers a globally-used video conferencing application, saw its sales jump by 326% in 2020 (BBC, 2021). This rise in Zoom’s adoption by both companies and the general public is largely attributed to the quarantine and isolation requirements of the global COVID-19 pandemic. Funerary live streaming services also saw a rise in adoption. James Montgomery of One Room Streaming, a popular funerary live streaming service, told NPR that the company has seen “a jump in the number of funeral homes using and requesting the service” (Eng, 2020).
3 “Several studies noted the unknown long-term consequences for family members who had lost someone close during the COVID-19 pandemic. Complicated or prolonged sorrow might be an increasing mental health problem due to the limited possibilities to understand and be involved in the care of a dying family member (Sizoo, et al., 2020; Heath, et al., 2020)” (Hugelius, et. al., 7).
4 Many different journal articles investigate multimodal digital rehabilitation and healthcare tools in this time when isolation and restrictions are needed to contain the COVID-19 pandemic. While one bibliometric analysis published in Frontiers in Public Health offered a number (3,194 articles), this number spans 2010 to 2020 (Xue, et al., 1). Though it is difficult to offer a discrete number without a similar bibliometric analysis, the number of relevant articles found in my research on digital health tools developed in response to COVID-19 was significant (over 300 relevant articles found).
Works Cited
1 In the cited article from the International Journal of Nursing Studies, the authors wrote that their research included data from (in no particular order) the United States, Saudi Arabia, Spain, Canada, France, India, the United Kingdom, the Netherlands, Italy, Taiwan, Hong Kong, Japan, Ireland, and Germany (Hugelius, et al., 3).
2 Zoom, the company that offers a globally-used video conferencing application, saw its sales jump by 326% in 2020 (BBC, 2021). This rise in Zoom’s adoption by both companies and the general public is largely attributed to the quarantine and isolation requirements of the global COVID-19 pandemic. Funerary live streaming services also saw a rise in adoption. James Montgomery of One Room Streaming, a popular funerary live streaming service, told NPR that the company has seen “a jump in the number of funeral homes using and requesting the service” (Eng, 2020).
3 “Several studies noted the unknown long-term consequences for family members who had lost someone close during the COVID-19 pandemic. Complicated or prolonged sorrow might be an increasing mental health problem due to the limited possibilities to understand and be involved in the care of a dying family member (Sizoo, et al., 2020; Heath, et al., 2020)” (Hugelius, et. al., 7).
4 Many different journal articles investigate multimodal digital rehabilitation and healthcare tools in this time when isolation and restrictions are needed to contain the COVID-19 pandemic. While one bibliometric analysis published in Frontiers in Public Health offered a number (3,194 articles), this number spans 2010 to 2020 (Xue, et al., 1). Though it is difficult to offer a discrete number without a similar bibliometric analysis, the number of relevant articles found in my research on digital health tools developed in response to COVID-19 was significant (over 300 relevant articles found).
Works Cited
- Casert, R., & Charlton, A. (20 April 2020). Nations seek to ease nursing home loneliness yet keep safe. AP News; The Associated Press. https://apnews.com/article/virus-outbreak-belgium-health-ap-top-news-international-news-a6050b9bde6e776f8d0989812d9d74f0
- Dobler, Robert. “Ghosts in the Machine: Mourning the MySpace Dead.” Folklore and the Internet: Vernacular Expression in a Digital World, edited by Trevor J. Blank, University Press of Colorado, 2009, pp. 175–93, https://doi.org/10.2307/j.ctt4cgrx5.11.
- Eng, Monica. “Social Distancing Means Mourners Find New Ways To Cope And Connect” NPR, NPR, 2 April 2020, https://www.npr.org/2020/04/02/825175482/social-distancing-means-mourners-must-find-new-ways-to-cope-and-connect
- Jewitt, Carey, et al. “Manifesto for Digital Social Touch in Crisis.” Frontiers in Computer Science, vol. 3, 25 Oct. 2021, 10.3389/fcomp.2021.754050. Accessed 10 Jan. 2022.
- Hugelius, Karin, et al. “Consequences of visiting restrictions during the COVID-19 pandemic: An integrative review.” International journal of nursing studies vol. 121 (2021): 104000. doi:10.1016/j.ijnurstu.2021.104000
- Vitaliano, Peter P., et al. “Is Caregiving a Risk Factor for Illness?” Current Directions in Psychological Science, vol. 13, no. 1, 2004, pp. 13–16. JSTOR, www.jstor.org/stable/20182897.
- Walker, Alexis J., et al. “Informal Caregiving to Aging Family Members: A Critical Review.” Family Relations, vol. 44, no. 4, 1995, pp. 402–411. JSTOR, www.jstor.org/stable/584996.
- Seppala, Emma, et al. “Social Connection and Compassion: Important Predictors of Health and Well-Being.” Social Research, vol. 80, no. 2, 2013, pp. 411–430. JSTOR, www.jstor.org/stable/24385608.
- Socolovsky, Maya. “Cyber-Spaces of Grief: Online Memorials and the Columbine High School Shootings.” JAC, vol. 24, no. 2, JAC, 2004, pp. 467–89, http://www.jstor.org/stable/20866634.
- World Health Organization (WHO). (1 June 2020). Maintaining essential health services: operational guidance for the COVID-19 context: interim guidance, 1 June 2020. https://apps.who.int/iris/handle/10665/332240
- Xue, Xiali et al. “Global Trends and Hotspots in Research on Rehabilitation Robots: A Bibliometric Analysis From 2010 to 2020.” Frontiers in public health vol. 9 806723. 11 Jan. 2022, doi:10.3389/fpubh.2021.806723
- “Zoom Sees More Growth after 'Unprecedented' 2020.” BBC News, BBC, 1 Mar. 2021, https://www.bbc.com/news/business-56247489.
About the Author
Smita Sen is an artist working with sculpture, dance-based performance, and advanced technology to research how the body internalizes its environment and significant life events. Sen’s work has been shown at Recess (Brooklyn, NY), Bard College (Annandale-on-Hudson, NY), Flux Factory (Long Island City, NY), and more. Smita has taught and designed the Emerging Media program at Choate Rosemary Hall. Sen’s most recent project, the Manipura Sanctum offers a meditative lens on caregiving and grief in times of illness and is on view at the Brooklyn Public Library’s Central branch in Grand Army Plaza through April 23rd, 2022.